The Provincial Health Services Authority (PHSA) delivers specialized health programs and services that are vital to the well-being of patients across British Columbia. As a key part of BC’s healthcare landscape, PHSA collaborates with the Ministry of Health and other health authorities to enhance the patient experience, ensure equitable access to care, and drive system-wide improvements for all British Columbians.
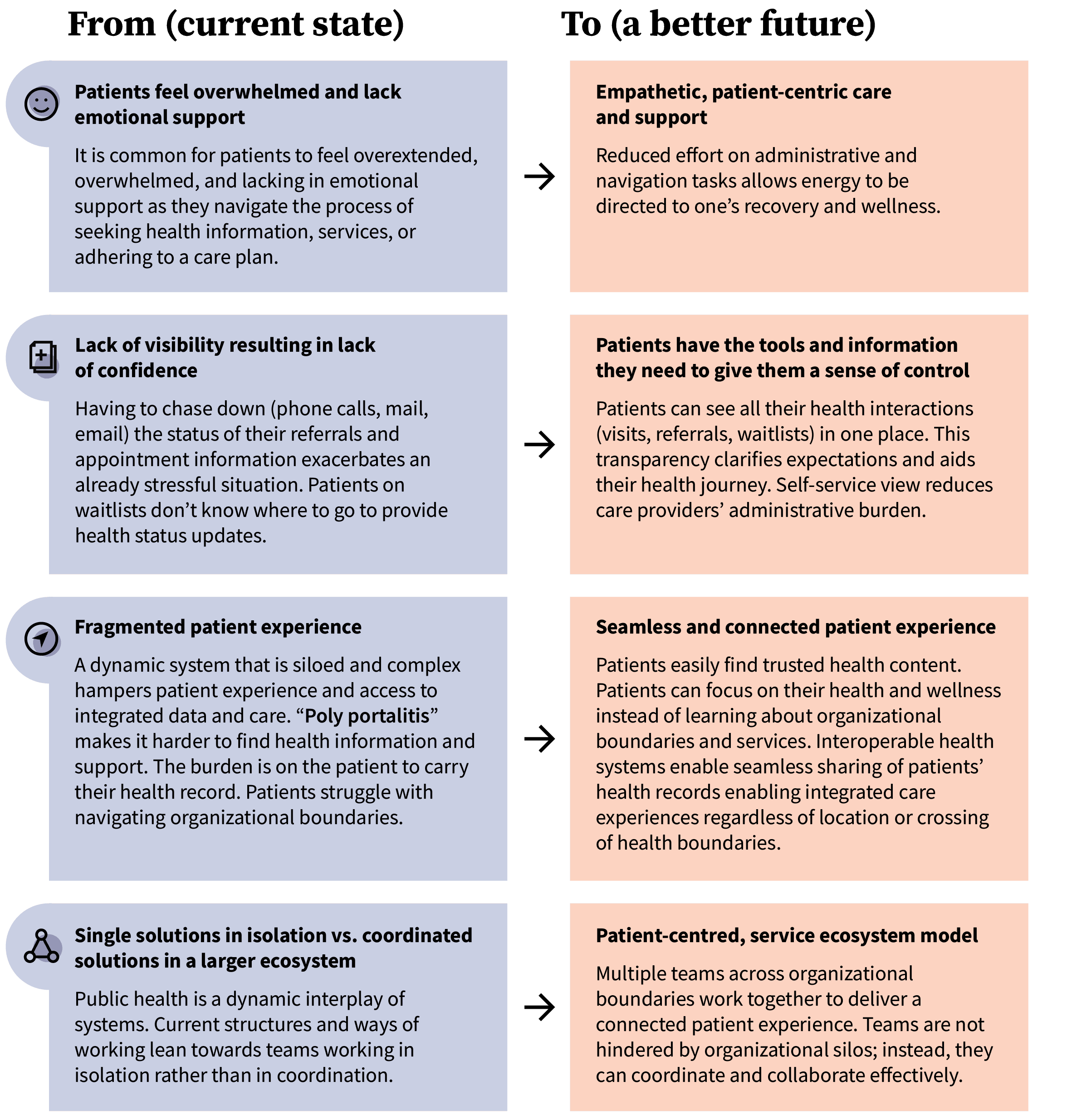
As with many health systems, a significant obstacle has persisted within British Columbia’s healthcare landscape: a fragmented patient experience.
Navigating a disconnected system
This fragmentation manifests as a complex healthcare system where patients and healthcare providers in BC face significant challenges navigating its complexities. Learning where to go, what to ask, and what actions to take can be overwhelming. As patients transition between different healthcare providers and health authorities, they often need to repeat their health history. This repetition stems from data dispersed across multiple online portals, providers’ records, and health information systems. This limits patients’ control over their health information and impacts providers, who may only have access to part of a patient’s medical history. As a result, patients experience a healthcare journey that feels broken and disconnected instead of smooth and supportive. Although steps are being taken to improve the often fragmented and siloed patient experience, additional efforts are necessary.
Using a collaborative approach to address challenges and opportunities
To tackle the challenges of inconsistent access to health information, digital disparities, and the complicated process of navigating multiple online portals and various providers, Provincial Digital Health—Ministry of Health and PHSA Digital—brought together patients, providers, and sector partners. We believe the best solutions emerge from those who use and deliver the service. That’s why OXD’s Service Design team took a collaborative, cross-sector, and patient-centred approach to truly understand and integrate diverse experiences.
We co-designed and developed a shared vision for a Connected Patient Experience (CPE) with over 60 digital and ministry leaders and patient representatives. This case study uses the term CPE project partners to refer to patients, providers, and sector partners who participated in a multitude of activities to define the vision for a Connected Patient Experience.
Applying a systems lens
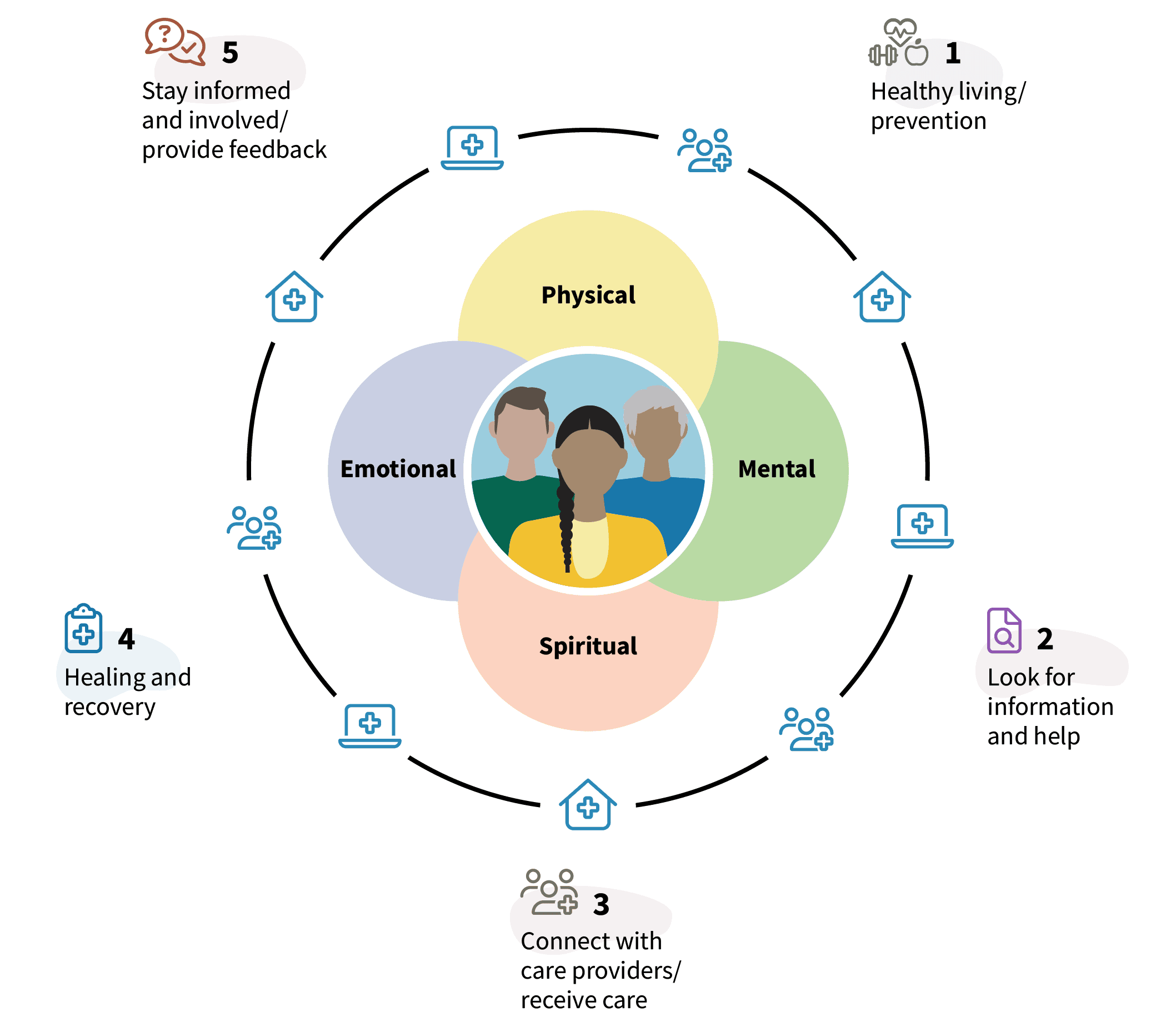
Our approach leveraged a systems lens, which addresses complex public sector challenges by understanding the interconnectedness of human, technological, organizational, and societal elements within public health—rather than focusing on isolated parts or events. This aligns with the BC government’s digital plan, specifically Mission 1: Connected Services, which highlights the need for connected services.
When designing new solutions, especially for wicked problems, we believe that true change happens when everyone involved helps shape it. No single team, organization or individual can tackle today’s complex challenges on their own. It necessitates co-design with the people responsible for implementing change and making design decisions. Healthcare professionals and administrative staff are essential contributors, as their processes—both digital and non-digital—significantly influence the feasibility of implementing a service and the overall patient experience. Although these individuals may not own the entire system, they play a crucial role and are most affected by any new design or intervention. While a successful future will naturally look different for each person, our aim was to foster alignment and build a path forward that benefits the entire system.
a. Starting with understanding the system via lived experiences
To envision the future possibilities for a Connected Patient Experience, we first needed a clear understanding of the present situation. We started by interviewing patients, providers, and health sector partners. Additionally, we held a patient experience mapping workshop to create a shared understanding of the current state and the challenges faced within it.
Mapping the current patient experience helped individuals see their respective parts of the service and helped CPE project partners come to a shared understanding of the “bigger picture” of the service as a whole. This mapping process provided a visual representation that teams used to identify pain points, redundancies, and areas of friction. These insights helped achieve alignment and consensus on the current pain points and served as inspiration for envisioning a better patient experience.
b. Imagining what good looks like
When working with a diverse group, there are often multiple perspectives and opinions around a desired future. Reaching a consensus on the vision for a Connected Patient Experience can be challenging due to conflicting motivations and differing goals and priorities. To explore these perspectives we brought together patients, providers, and sector partners to contemplate and discuss:
- How do we define a “Connected Patient Experience”?
- What future do we hope to build, and what outcomes do we expect to see?
- What kind of value could be delivered, and for whom?
Through this collaborative process, participants were able to see the project’s potential from each other’s point of view. This collective effort helped them envision a shared future and identify how different forms of value could be realized. In a large-scale system such as health, multiple beneficiaries can derive value from a Connected Patient Experience.
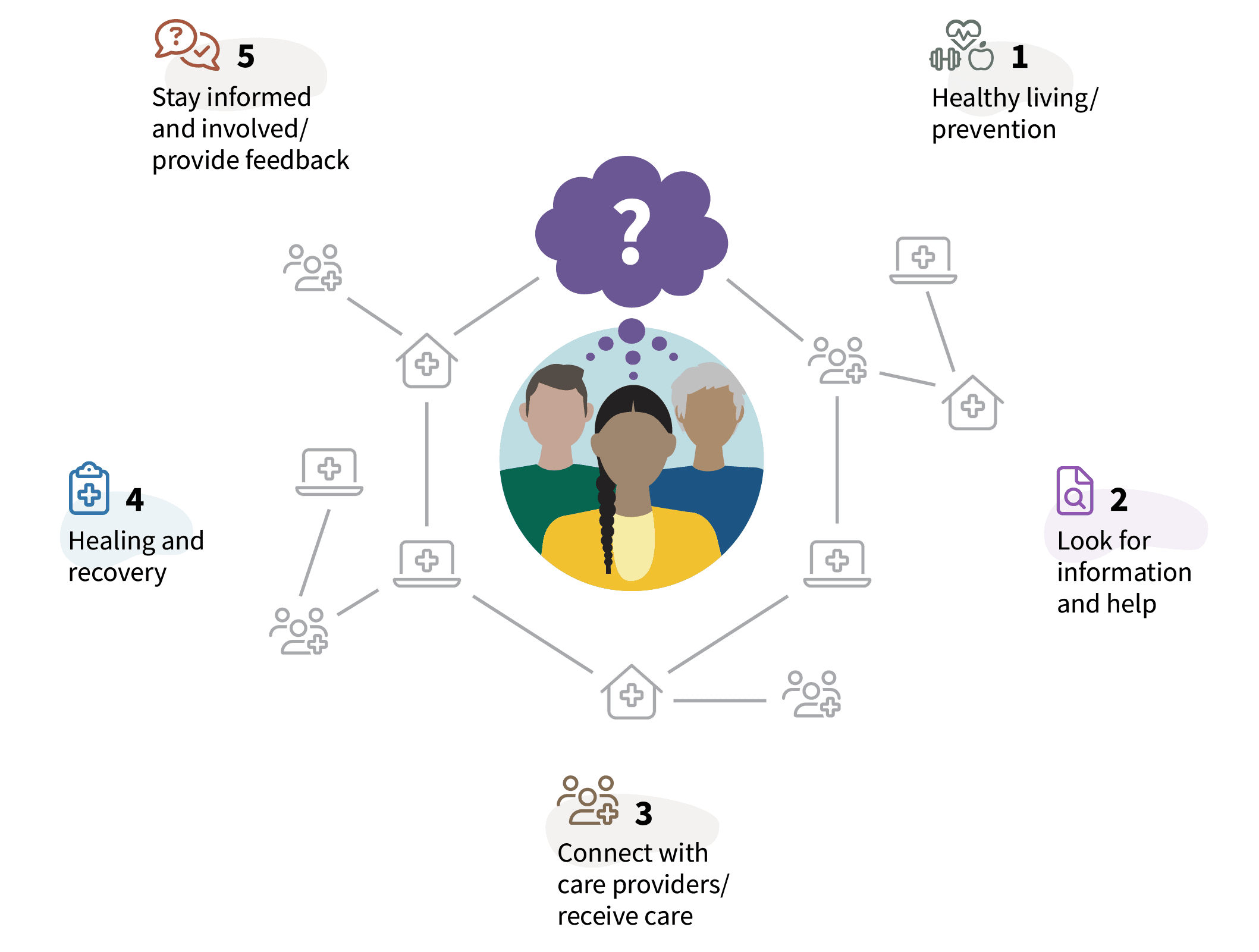
c. Imagining future possibilities of a Connected Patient Experience
Once we defined the potential value and outcomes for a Connected Patient Experience we could begin to define the necessary interventions. This involved identifying the processes, policies, tools, technology, and people required to design, enable, and deliver a truly connected experience for patients.
To provide a reference point, a preliminary CPE outcomes statement was drafted:
The Connected Patient Experience aims to ensure that patients have the autonomy to access and act on their health information, while creating multimodal patient engagement strategies that address inequities contributing to the digital divide. It also seeks o promote cross-sector collaboration and coordination of a quality digital patient experience to access health information and interactive services along their journeys. This will help to address fragmentation of the digital user experience to increase access to care, improve patient satisfaction and outcomes, and reduce administration burden on providers.
We asked workshop participants:
- How might we support this outcome statement? What possibilities lie ahead for a Connected Patient Experience?
- How might we leverage our diversity of experiences, skills, and capabilities to design, implement, and sustain a Connected Patient Experience?
Workshop attendees worked in small groups capturing their tactical ideas in a mad-lib-type worksheet.
Since every challenge has multiple solutions, we set out to imagine many possibilities and interventions for the future. Striving for a single, “perfect” future solution is often unrealistic and limiting. Multiple solutions are possible and necessary because we operate within diverse social systems simultaneously. Considering various future options helps us avoid groupthink and unlocks the potential for more novel, innovative, and impactful solutions.
d. Coalescing and articulating the vision statement for a Connected Patient Experience
Thanks to the generosity of patients, providers, and health sector partners who contributed their time and engaged in various co-design activities, we were able to craft a unified CPE vision. A comprehensive understanding of various ideas, hopes, fears, and potential futures has shaped the vision statement for the Connected Patient Experience. This statement is the “why” for change.
Connected Patient Experience vision
Aligning with the first three pillars of BC’s Digital Health Strategy, the CPE vision aims to establish a connected health system that empowers patients in their healthcare and improves provider experiences.
People can access health information and services no matter how they enter the health system. Interoperable health systems facilitate seamless sharing and access to patients’ health information. An appropriate balance of culturally safe person-to-person and digitally delivered services to support varying degrees of digital literacy and access.
“The new vision follows a user-centred service design approach and builds upon a sophisticated and scalable digital healthcare architecture.”
Danton Remacle, Senior Director, Service Design and Patient Empowerment
This vision now serves as a shared guiding purpose for everyone involved in designing, delivering, and supporting healthcare in British Columbia.
e. From vision to reality: Identifying key changes
Defining a vision is just the first step. The next challenge lies in figuring out how to get started and measure progress. CPE project partners identified potential conditions and barriers to achieving the CPE vision. While this vision directs our collective efforts, we identified several critical shifts that must occur to turn it into reality. These shifts are essential changes in how organizations, teams, or individuals operate, transforming current practices into a more effective future state. They serve as foundational building blocks, guiding the creation of products, services, and experiences that align directly with the CPE vision. Some of the shifts identified for realizing the CPE vision include:
Achieving alignment: A path forward for patient care
Building shared understanding and agreement among diverse participants can be a significant challenge in any large-scale initiative. Through a comprehensive, collaborative, patient-centred, cross-sector approach, Provincial Digital Health and all involved have successfully established:
- A unified, province-wide vision for a Connected Patient Experience that delivers on BC’s Digital Plan while improving efficiency and patient satisfaction. This unified vision defines a future where patient interactions with the healthcare system are seamless and supportive, regardless of the entry point.
- Emerging tactical strategies for creating and supporting a connected patient experience through integrated service offerings rather than isolated technological solutions and data silos.
To solve complex public sector challenges effectively, our approach championed deep collaboration. We used structured activities to break down internal silos and organizational boundaries, taking a holistic view of the system. Recognizing that change efforts often involve varied perspectives, we focused on unifying involved parties around shared values and aspirations. The resulting shared vision serves as a unified purpose for everyone involved in designing, delivering, and supporting healthcare across the province.
Enacting and living the vision
To drive and realize the CPE vision, PHSA has established a CPE Strategic Planning Council. The CPE Council is composed of patient advisors, healthcare providers, and sector partners from across the province who advise on key provincial patient-facing digital initiatives and priorities. The council meets each month, providing a valuable forum for members to share insights, discuss ongoing initiatives, and explore collaborative opportunities.
As noted earlier, no single team, organization or individual can tackle today’s complex challenges independently. Moving forward, sustained engagement with patients, front-line providers, and collaborative dialogue across leadership levels of ministries and health authorities will be essential.